 In 2017, the suicide rate reached a 33-year high. Suicide is now the second-leading cause of death among teenagers, and an American dies by suicide every 12.8 minutes.
In 2017, the suicide rate reached a 33-year high. Suicide is now the second-leading cause of death among teenagers, and an American dies by suicide every 12.8 minutes.
Deaths by suicide are often surrounded by unanswered questions. Those left behind may feel a combination of grief, guilt, anger, and confusion. People experiencing suicidal thoughts often struggle to feel heard. Myths about suicide, such as the idea that talking to a suicidal person can make them more suicidal, are pervasive.
Suicide is a preventable tragedy. Knowing what to say and what to do when someone is having thoughts of suicide can save lives. The way we talk about suicide matters, and the effects of these discussions extend far beyond conversations with loved ones. Research suggests the way journalists write about suicide can increase the suicide rate. A constructive approach to reporting on and talking about suicide raises awareness and cultivates empathy without sensationalizing death.
Why We Need to Talk About Suicide
“One of the biggest misconceptions around suicide is that talking about it will cause it,” said Lisa Danylchuk, LMFT. Danylchuk is an Oakland, California, therapist who specializes in treating trauma survivors. She often works with people experiencing suicidal thoughts.
People who talk about suicide are not doing it to get attention. Bringing up suicide can be very difficult, so if someone broaches the topic of suicide, it suggests they want help. Suicide is rarely impulsive, and many people who die by suicide first discussed it with a loved one.People concerned about a loved one’s emotions should consider broaching the topic of suicide. Initiating a discussion does not implant the idea. Instead, it can provide a safe space to talk about stigmatized feelings.
“Giving people a space to explore their feelings related to suicide often helps them process their feelings,” Danylchuk said. “It also helps those concerned to monitor the severity of suicidal ideation and reach out for the appropriate support when necessary.”
The American Foundation for Suicide Prevention (AFSP) offers a basic primer on the benefits of talking about suicide. Talk Saves Lives organizes brief presentations in communities across the nation to help people recognize the warning signs of suicide and learn how it can be prevented.
Reporting on Suicide: The Contagion Effect
Talking about suicide does not cause suicide, but reporting on it might. Articles and stories about suicide can create a contagion effect, potentially pushing people who are already at risk of suicide to more seriously consider it. Suicide prevention experts call this the Werther Effect, named for the novel The Sorrows of Young Werther by Johann Wolfgang von Goethe. After the 18th century publication of the novel, young men began imitating its protagonist. Some copied his suicide and suicide method. Some areas banned the novel in an attempt to save lives.
Researchers have observed a contagion effect associated with glamorized and heavily publicized suicide ever since.
“We have more than 100 studies from around the world now that demonstrate how media reports on suicide impact the risk of contagion,” said Daniel Reidenberg, PsyD, the executive director of Suicide Awareness Voices of Education (SAVE). “The more frequently a story is reported on, the placement of the story in a newscast or in print, the more graphic and sensational a story—all impact the audience. We know that when suicide is romanticized or glorified, that too leads to suicide contagion. When someone is memorialized in the media, some believe they too will be just like the person they are seeing in the news, and that gives them an identity or recognition that they don’t necessarily feel.”
Reidenberg trains journalists who report on suicide, and he helped develop a list of best practices for journalists reporting on suicide. He says most journalists do not understand their role in contagion, yet simple changes in the way journalists talk about suicide can make a big difference. A 2007 study of Austrian guidelines for reporting on suicide found use of the guidelines lowered the nation’s suicide rate by 80% in just six months.
Guidelines for Reporting on Suicide
Reidenberg says media outlets tend to rely on stereotypes and clichés when reporting on suicide, but he cautions that suicide is never because of a breakup or a bad grade in school. Multiple factors figure into the decision for someone to take their own life. Reports that gloss over this nuance make it seem like a single bad event is enough to lead to suicide.
Likewise, reports that focus only on positive characteristics of the person who died can glamorize suicide. People who feel hopeless might think they will be remembered in the same way. The same is true for reports that highlight loved ones’ reactions.
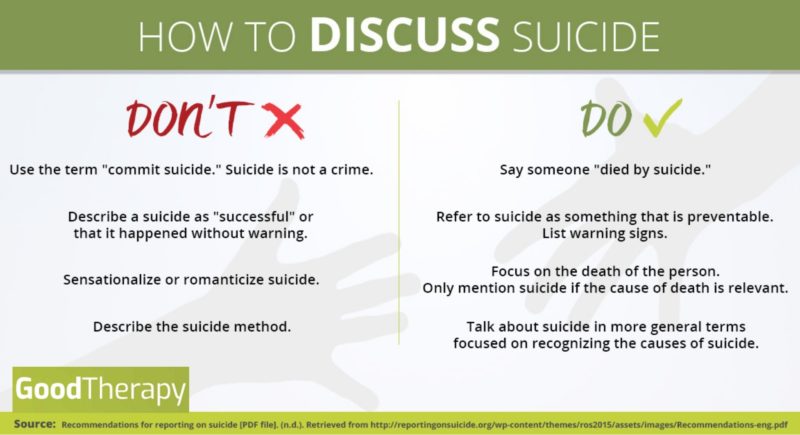
Experts make the following recommendations to journalists reporting on suicide:
- Avoid sensationalized headlines that focus on suicide or the method of death. Report the facts instead, and avoid using suicide as an attention-grabbing topic.
- Use neutral photos, such as school pictures, rather than images of bereaved family.
- Include contact information for a suicide hotline.
- Avoid hyperbolic language such as “suicide epidemic.” Use specific language such as “rise in the suicide rate.”
- Don’t use “successful” to refer to a completed suicide.
- Don’t characterize a suicide as sudden or without warning, and don’t focus on a single precipitating factor, such as a job loss. Instead, include a list of warning signs and intervention tactics.
- Don’t highlight or provide excerpts from a suicide note.
- Don’t treat suicide as criminal or report on it in a manner similar to criminal acts. Focus on suicide as a public health concern.
- Don’t interview or quote police or first responders. Instead, ask suicide prevention or mental health experts for insight.
- Don’t describe the method of suicide, particularly not in graphic detail.
These guidelines reduce the likelihood that vulnerable people will see suicide as thrilling, glamorous, or the inevitable result of a sudden difficulty. They also help reporters avoid victim blaming and reduce stigma by treating suicide as a health concern, not a moral or criminal issue.
How to Talk to a Suicidal Person
“We know that it is okay to talk about suicide, even with someone who might be thinking about it,” Reidenberg said. “Doing so does not make them want to die more or lead them to attempt suicide. In fact, talking with someone who is thinking about this can reduce their level of anxiety, distress, and hopelessness and encourage them to seek help. Research shows that if you’re worried about someone, talk to them. It’s okay to do that.”
Danylchuk echoed these sentiments, suggesting a simple aphorism: “When in doubt, talk it out.”
Yet, talking to a suicidal person can be intimidating. Together Strong, an organization and app that helps veterans adjust to civilian life after deployment, suggests beginning the conversation directly, without judgment. Make an observation about recent behavior, or ask an open-ended question about how the person is feeling.
Don’t talk about how the person is making you feel, and don’t judge their behavior. This shuts down conversation, and can increase feelings of frustration and hopelessness. “You’re stressing me out with your negativity” is unhelpful. “I’ve noticed you seem sad lately. How are you feeling?” is more effective.
When a person shares their feelings of hopelessness or thoughts of suicide, try the following strategies:
- Validate their feelings. It may be tempting to minimize their suffering in an attempt to get them to change their suicidal thoughts. Validation, however, can help your loved one feel understood. It encourages them to keep talking. Talking can save lives.
- Don’t act shocked, angry, or disappointed. It can be difficult to talk about suicide, and these reactions shut down the discussion.
- Listen attentively, and avoid rushing your loved one or appearing annoyed.
- Know that people contemplating suicide often have mental health issues. Your loved one might say things that don’t make sense or that you dislike. Avoid judging or labeling them.
- Take talk of suicide seriously. Never suggest a person take their life in a moment of your own exasperation. Never suggest they are only seeking attention.
- Allow your loved one to freely express their emotions in a way that works for them. Don’t judge or shame them for using profanity, questioning deeply held spiritual beliefs, expressing anger at loved ones, or saying something that shocks you.
- Ask the person if there is something they need or something you can do to help. This allows them to ask for something—a ride to the emergency room or companionship, for example—if they need it. Be prepared for them to say no or that they don’t know, but don’t end the conversation there.
- Ask your loved one if they can think of reasons to live. Devising a list of reasons to live can reduce the power of suicidal feelings. If your loved one is unable to devise such a list, don’t judge, argue with, or shame them.
Preventing Suicide
When someone expresses suicidal thoughts or feelings, remaining engaged in a conversation is a powerful antidote. People who are able to talk have an outlet for their pain. Companionship and conversation can be temporary antidotes to thoughts of suicide.
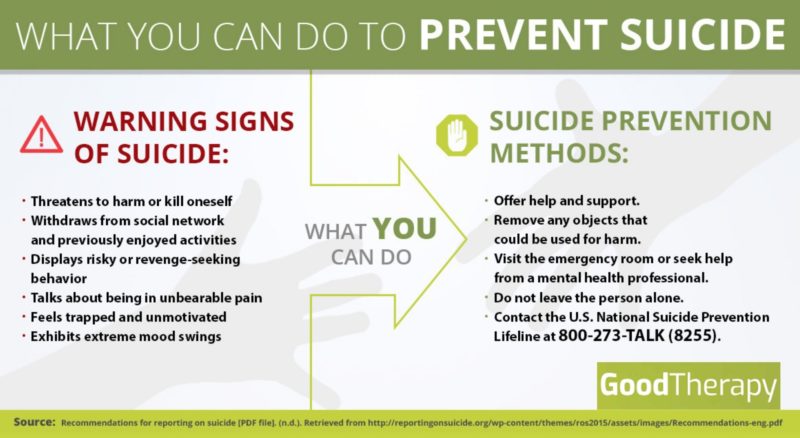
To further reduce the risk:
- Do not leave a person experiencing suicidal thoughts alone. If you can’t be with them, find someone who can, such as a parent, a friend, or other loved one.
- Call a suicide hotline. The person on the other end of the line can connect you to emergency intervention services in your area, offer you the support you need to be a good listener, and answer questions about suicide. The National Suicide Prevention Lifeline offers an online chat, or you can call 1-800-273-8255 for help over the phone.
- Don’t agree to keep someone’s thoughts of suicide secret, but don’t use a person’s feelings to humiliate them. Share their feelings with someone who is equipped to help. That person might be a parent, sibling, or loved one. It could also be a mental health expert. The right person varies. For example, a teacher worried about a suicidal teenager with abusive parents should consider talking to someone other than the teen’s parents.
- Remove objects the person could use to hurt themselves, such as drugs or weapons.
- Ask the person if they can agree not to kill themselves for a short period of time. Encourage them to give it a day, a week, or even an hour. This can be particularly helpful if you cannot be in physical contact with the person or if they are waiting to receive mental health care.
- Encourage the person to go to the emergency room or to a crisis mental health facility. If you can, offer to go with them so they feel less alone.
- Contact an emergency service. Call 911 or an ambulance if you believe the person is in immediate danger or if they have already attempted suicide. In some regions, the police have suicide intervention training. In other regions, mobile mental health crisis services are available. Researching options ahead of time can help you know what number to call.
- Contact your local chapter of the National Alliance on Mental Illness (NAMI). NAMI provides resources and support to people who love someone who is experiencing mental health issues.
Suicide Warning Signs
While some people experiencing suicidal thoughts may openly share these thoughts, others may suffer in silence. The AFSP highlights the following warning signs:
- Talk of feeling trapped, being a burden, having no reason to live, or facing unbearable pain
- Changes in mood, including increases in anxiety, depression, anger, loss of interest in life, or feelings of shame and humiliation
- Reckless behavior, including aggression or increased use of drugs or alcohol
- Giving things away
- Isolating oneself from loved ones, or reaching out to people to say goodbye
Mental health issues such as depression and anxiety are significant risk factors for suicide. People who express suicidal feelings who have access to a weapon, or who have a clear plan or suicide method, are at a heightened risk. Some other risk factors for suicide include:
- Experiencing a stressful life event, though no single factor causes suicide
- Experiencing prolonged stress, such as bullying or a chronic illness
- Exposure to another person’s suicide, such as the suicide of a classmate, or to sensationalized reports of suicide
- Previous suicide attempt
- A family history of suicide
Suicide is preventable, and bystanders can help. If you need help for yourself or someone you love, you can call the following phone numbers for help:
- National Suicide Prevention Lifeline: 1-800-273-8255
- NAMI HelpLine: 1-800-950-6264
- Trans Lifeline: 1-877-565-8860
- National Center for Posttraumatic Stress Disorder Veterans Crisis Line: 1-800-273-8255, ext. 1
- Mental Health America (for area-specific referrals): 1-800-969-6642
- Postpartum Support International (for general information, not crisis intervention): 1-800-994-4773
- National Sexual Assault Hotline: 1-800-656-4673
References:
- Increase in suicide in the United States, 1999-2014. (2016, April 22). Retrieved from https://www.cdc.gov/nchs/products/databriefs/db241.htm
- Kirkwood, A. (n.d.). Tips for talking to students about suicide [PDF]. Oregon Youth Suicide Prevention Campaign.
- Niederkrotenthaler, T., Herberth, A., & Sonneck, G. (n.d.). The ‘Werther-effect’: Legend or reality? Neuropsychiatry, 21(4), 284-290.
- Suicide: 2016 facts and figures [PDF]. (2016). American Foundation for Suicide Prevention.
- Suicide claims more lives than war, murder, and natural disasters combined. (n.d.). American Foundation for Suicide Prevention. Retrieved from https://afsp.donordrive.com/index.cfm?fuseaction=cms.page&id=1226&eventGroupID=9AA19459-C880-0E26-61312B15147B2E0A&cmsContentSetID=D5C4DC12-C299-258B-B0B6FCF9EF015CE0
- Suicide prevention: Myth or fact? (n.d.). Retrieved from http://ucc.nd.edu/self-help/depression-suicide/suicide-prevention-myth-or-fact/
- Suicide statistics. (n.d.). American Foundation for Suicide Prevention. Retrieved from https://afsp.org/about-suicide/suicide-statistics
- Tips and tactics: Recognizing red flags [PDF]. (2014). Together Strong.
- VanOrman, A., & Jarosz, B. (2016, June). Suicide replaces homicide as second-leading cause of death among U.S. teenagers. Retrieved from http://www.prb.org/Publications/Articles/2016/suicide-replaces-homicide-second-leading-cause-death-among-us-teens.aspx

The preceding article was solely written by the author named above. Any views and opinions expressed are not necessarily shared by GoodTherapy.org. Questions or concerns about the preceding article can be directed to the author or posted as a comment below.


 Suicide and Saying Goodbye: Leaving Survivors with Love
Suicide and Saying Goodbye: Leaving Survivors with Love What We Mean When We Talk About Suicide
What We Mean When We Talk About Suicide Suicide in the Spring: Practice Prevention as Seasons Change
Suicide in the Spring: Practice Prevention as Seasons Change

Please fill out all required fields to submit your message.
Invalid Email Address.
Please confirm that you are human.
Leave a Comment
By commenting you acknowledge acceptance of GoodTherapy.org's Terms and Conditions of Use.